achilles tendon rupture rehab exercises pdf
Achilles tendon rupture rehab exercises are crucial for restoring strength, flexibility, and function. A structured program, including stretching, strengthening, and progressive loading, promotes optimal recovery and prevents reinjury.
1.1 Understanding the Importance of Rehabilitation
Rehabilitation is critical after an Achilles tendon rupture to restore strength, flexibility, and function. A well-structured program prevents chronic pain, limited mobility, and future injuries. Proper exercises promote tendon healing, improve joint mobility, and strengthen surrounding muscles. Without rehabilitation, patients may face long-term disability or recurring issues. Early intervention ensures faster recovery and a return to daily activities. Consistency and adherence to a rehab plan are vital for optimal outcomes and preventing reinjury. Understanding the importance of rehabilitation helps patients commit to the process, ensuring a safer and more effective journey toward full recovery.
1.2 Overview of Achilles Tendon Rupture
An Achilles tendon rupture is a complete or partial tear of the tendon connecting the calf muscles to the heel bone. It often occurs due to sudden movement or overuse, causing pain, swelling, and difficulty walking. Symptoms include a snapping sound at the time of injury, inability to stand on tiptoes, and bruising. Treatment options vary, with surgery or non-surgical approaches depending on severity and patient activity level. Early diagnosis is crucial for effective recovery. Even without surgery, rehabilitation is essential to restore tendon strength and prevent further injury. Understanding the injury’s nature helps guide appropriate treatment and rehab strategies.
1.3 Role of Exercises in Recovery
Exercises play a pivotal role in Achilles tendon rupture recovery, promoting healing, strength, and flexibility. They help restore mobility, reduce stiffness, and prevent muscle atrophy. Early exercises focus on gentle movements to avoid re-injury, progressing to strengthening activities like calf raises and heel drops. These routines enhance tendon repair, improve joint stability, and rebuild muscle function. Consistency in exercise ensures gradual loading of the tendon, fostering resilience. Additionally, exercises address psychological recovery by empowering patients with active participation in their healing process. A well-structured exercise program is essential for achieving full recovery and returning to normal activities. Proper progression ensures long-term durability and function of the tendon.

Immediate Post-Injury Care
Immediate post-injury care for Achilles tendon rupture involves immobilization, pain management, and early mobility practices to protect the tendon and promote initial healing, preventing further damage.
2.1 Immobilization Techniques
Immobilization is critical immediately after an Achilles tendon rupture to prevent further damage and promote healing. Common methods include casts, braces, or splints to keep the tendon stable. A walking boot or orthopedic shoe with a raised heel can also be used to minimize stress on the tendon. Immobilization typically lasts 4-6 weeks, depending on the severity of the injury. Proper fitting of these devices is essential to avoid complications like pressure sores or restricted blood flow. This period of immobilization is vital for allowing the tendon to begin the healing process before progressing to weight-bearing activities or exercises.
2.2 Pain Management Strategies
Effective pain management is essential during the early stages of Achilles tendon rupture recovery. Over-the-counter pain relievers like ibuprofen or naproxen can help reduce inflammation and alleviate discomfort. Ice therapy, applied for 15-20 minutes several times a day, is also beneficial in minimizing swelling and pain. Elevation of the affected leg above heart level further reduces swelling. In some cases, prescription pain medication may be necessary, but it should be used cautiously and under medical supervision. Additionally, gentle compression bandages can provide support and reduce pain. It’s important to balance pain relief with gradual mobilization to avoid prolonged immobility, which can hinder recovery.
2.3 Early Mobility Practices
Early mobility practices are vital to prevent stiffness and promote healing after an Achilles tendon rupture. Gentle movements, such as heel slides and ankle pumps, can be performed while the tendon is immobilized. Partial weight-bearing exercises, using crutches or a walking boot, help maintain muscle strength without overloading the tendon. Gradual mobilization under the guidance of a physical therapist ensures safe progression. These practices aim to restore range of motion, reduce muscle atrophy, and prepare the tendon for more advanced exercises. Early mobility must be balanced with rest to avoid reinjury, making it a critical component of the rehabilitation process.

Phases of Achilles Tendon Rehab
Achilles tendon rehab is divided into four phases: initial healing, strengthening, advanced strengthening, and return to activity. Each phase targets specific recovery goals to ensure proper tendon repair and functional restoration.
3.1 Phase 1: Initial Healing (0-4 weeks)
Phase 1 focuses on protecting the tendon and promoting natural healing. Immobilization with a brace or boot is essential to minimize stress on the tendon. Pain management strategies, such as ice therapy and anti-inflammatory medications, are implemented to reduce discomfort. Gentle exercises, like ankle pumps and heel raises, are introduced to maintain joint mobility without risking further injury. This phase lays the foundation for recovery, ensuring the tendon begins to repair itself before progressing to more active movements. Strict adherence to immobilization and activity modification is crucial during this period to avoid reinjury.
3.2 Phase 2: Strengthening (4-8 weeks)
Phase 2 focuses on gradually increasing strength and load on the Achilles tendon. Resistance band exercises, calf raises, and heel lifts are introduced to rebuild muscle strength and tendon integrity. Weight-bearing activities are progressed carefully, ensuring the tendon can tolerate stress without pain. This phase also emphasizes controlled movements to improve functional mobility. Patients may begin using a brace with adjusted tension to support the tendon during exercises. The goal is to restore sufficient strength for basic movements while avoiding overloading the tendon. Progression is slow and monitored to ensure proper healing and prevent setbacks.
3.3 Phase 3: Advanced Strengthening (8-12 weeks)
Phase 3 focuses on advanced strengthening, incorporating higher resistance and dynamic exercises. Activities like plyometrics, agility drills, and single-leg balance exercises are introduced to enhance tendon resilience and functional recovery. Resistance bands with increased tension and weighted calf raises challenge the tendon further. Patients progress to more complex movements, simulating real-life activities, to restore full mobility and strength. The use of balance boards or unstable surfaces improves proprioception and stability. This phase aims to prepare the tendon for higher demands, ensuring readiness for sport-specific or high-impact activities by gradually increasing intensity and complexity of exercises. Monitoring progress ensures a smooth transition to the next phase.
3.4 Phase 4: Return to Activity (3-6 months)
Phase 4 focuses on safely returning to pre-injury activities and sports. Patients gradually reintroduce high-level movements, such as sprinting, cutting, and jumping, with a emphasis on proper technique. Sport-specific exercises are tailored to mimic real-game scenarios, ensuring the tendon can handle dynamic stresses. Plyometric exercises, like box jumps and burpees, are advanced to rebuild explosive power. Balance and agility drills further refine functional stability. The goal is to restore full confidence and performance capacity while minimizing reinjury risks. Continuous monitoring and adjustments ensure a seamless transition back to full activity, with maintenance exercises recommended to sustain long-term tendon health and function.

Types of Rehab Exercises
Achilles tendon rehab includes stretching, strengthening, balance, and plyometric exercises. These promote tendon repair, improve flexibility, and restore functional movement, ensuring a full recovery and return to activity.
4.1 Stretching Exercises
Stretching exercises are essential in Achilles tendon rupture rehabilitation to restore flexibility and range of motion. Common stretches include calf stretches, heel drops, and plantar fascia stretches. These exercises target the gastrocnemius and soleus muscles, reducing stiffness and promoting tendon healing. Regular stretching helps improve ankle mobility, essential for daily activities and sports. Patients should perform stretches gently, avoiding pain, and hold each stretch for 20-30 seconds. Consistency is key, with exercises done 2-3 times daily. Over time, stretching lays the foundation for strengthening and functional movements, ensuring a successful recovery and reducing the risk of future injuries.
4.2 Strengthening Exercises
Strengthening exercises are vital for rebuilding Achilles tendon integrity and muscle function post-rupture. Early-stage exercises include heel raises, calf raises, and resistance band work to target the gastrocnemius and soleus muscles. Progression involves increasing resistance, such as using weights or incline boards. Functional exercises like step-ups and balance work enhance tendon loading and muscle coordination. Strengthening improves tendon resilience, reducing reinjury risk and restoring pre-injury activity levels. Consistency and gradual progression are key to avoiding overloading the tendon during recovery. These exercises form the foundation for advanced movements, ensuring a robust return to normal function and athletic performance.
4.3 Balance and Proprioception Exercises
Balance and proprioception exercises are essential for restoring stability and coordination after an Achilles tendon rupture. These exercises target the neuromuscular system, enhancing the body’s ability to sense movement and maintain equilibrium. Techniques include single-leg stands, wobble board training, and BOSU ball exercises. Progression involves adding challenges like eyes-closed balancing or dynamic movements. Proprioception drills, such as heel-to-toe walking and ankle disc exercises, further improve joint awareness and muscle activation. These exercises prevent compensatory patterns, reduce fall risk, and prepare the tendon for functional activities. Incorporating balance training ensures a more stable and resilient recovery, minimizing the risk of future injuries or chronic issues.
4.4 Plyometric and Agility Exercises
Plyometric and agility exercises are advanced rehab techniques aimed at restoring explosive power and dynamic movement after an Achilles tendon rupture. These exercises, such as box jumps, burpees, and lateral hops, simulate real-world activities and sports-specific movements. Agility drills, including cone drills and zigzag runs, improve quick changes of direction and coordination. Proper form and progression are critical to avoid overloading the tendon. Plyometrics enhance power and reactivity, while agility training refines speed and precision. These exercises are typically introduced in the later stages of rehab, preparing the individual for high-intensity activities and reducing the risk of reinjury during dynamic sports or daily tasks.
Exercise Progression
Exercise progression involves a tailored, gradual increase in intensity, duration, and complexity to optimize recovery. It ensures a smooth transition from basic rehab to advanced, functional movements safely.
5.1 Progression of Weight-Bearing Activities
Progression of weight-bearing activities is vital in Achilles tendon rupture rehabilitation to restore normal gait and function. It begins with non-weight-bearing exercises, advancing to partial weight-bearing with assistive devices like crutches or braces; As healing progresses, patients gradually transition to full weight-bearing activities, incorporating exercises like heel raises and single-leg stands. This phased approach ensures the tendon adapts to increasing loads without risking reinjury. Proper alignment, balance, and strength are emphasized to prepare the patient for daily activities and sports. The progression must be tailored to the individual’s healing stage and tolerance, ensuring a safe and effective return to full mobility.
5.2 Gradual Increase in Resistance
A gradual increase in resistance is essential for strengthening the Achilles tendon during rehabilitation. Resistance bands, weights, or progressive resistance exercises are commonly used to enhance tendon strength and muscle endurance. Initially, low resistance is applied to avoid overloading the tendon, with incremental increases as healing progresses. Exercises like calf raises and heel lifts are performed with added resistance to simulate real-world stresses. This method promotes tendon remodeling and improves functional capacity. Monitoring symptoms ensures resistance levels remain tolerable, preventing setbacks. The controlled progression of resistance helps achieve long-term durability and reduces the risk of reinjury, fostering a stable and effective recovery process.
5.3 Incorporating Functional Movements
Incorporating functional movements into Achilles tendon rehab is vital for restoring everyday and sports-specific activities. Exercises like gait training, balance drills, and single-leg stance work improve coordination and proprioception. Functional movements mimic real-life tasks, such as walking, running, and jumping, preparing the tendon for dynamic stresses. Agility drills and plyometric exercises are introduced in later stages to simulate high-impact activities. These movements enhance tendon strength, flexibility, and endurance, reducing the risk of reinjury. A physical therapist often guides the progression to ensure proper mechanics and safety. Gradually integrating functional movements ensures a smooth transition to normal activities, promoting long-term recovery and optimal performance.

Tools and Resources for Rehab
Resistance bands, balance boards, and physical therapy equipment are essential tools for Achilles tendon rehab, aiding in strength, stability, and guided exercises for optimal recovery.
6.1 Use of Resistance Bands
Resistance bands are versatile tools in Achilles tendon rehabilitation, offering adjustable tension for strengthening exercises. They are lightweight, portable, and cost-effective, making them ideal for both home and clinical settings. By anchoring the band or wrapping it around the foot, users can perform controlled movements that target the calf muscles and Achilles tendon. These exercises, such as plantar flexion and dorsiflexion, help restore strength and flexibility. Resistance bands also allow for progressive overload, enabling patients to gradually increase intensity as they heal. Their ease of use and effectiveness make them a cornerstone in many rehab programs, promoting safe and efficient recovery.
6.2 Balance Boards and Foam Pads
Balance boards and foam pads are essential tools for improving proprioception and stability during Achilles tendon rehabilitation. These devices create an unstable surface, challenging the lower leg muscles to maintain balance. Single-leg exercises on a balance board enhance ankle stability, while foam pads add texture for progressive difficulty. They help restore natural movement patterns, reducing reinjury risk. Incorporating these tools strengthens the calf muscles and tendon, promoting functional recovery. Their versatility allows for customization, making them ideal for gradual progression in rehab programs.
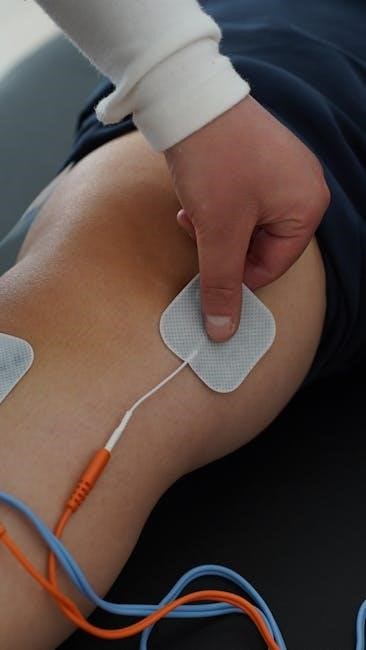
6.3 Role of Physical Therapy Equipment
Physical therapy equipment plays a vital role in Achilles tendon rehabilitation by providing targeted support and enhancing exercise effectiveness. Tools like stationary bicycles and elliptical machines facilitate low-impact mobilization, improving circulation and joint mobility. Ultrasound therapy machines promote tissue healing by stimulating blood flow and reducing inflammation. Traction devices and electrotherapy units may also be used to alleviate pain and strengthen the tendon. These technologies, combined with manual therapy techniques, accelerate recovery and ensure a safer return to functional activities. They are often integrated into structured rehab programs to optimize outcomes and minimize the risk of reinjury during the healing process.

Creating a Rehab Exercise PDF Guide
Creating a rehab exercise PDF guide involves organizing exercises clearly, adding images for better understanding, and providing step-by-step instructions for each activity.
7.1 Structuring the Guide
Structuring an Achilles tendon rupture rehab exercise PDF guide involves organizing content logically. Start with an introduction explaining the injury and recovery goals. Include sections for each rehab phase, detailing exercises with clear instructions and visuals. Use bullet points and headings for easy navigation. Add a progress tracker to monitor recovery milestones. Ensure the guide is user-friendly, with visuals to demonstrate proper form. Include a glossary of terms and a reference section for further reading. This structure helps patients follow the program effectively and stay motivated throughout their recovery journey.
7.2 Including Visual Aids and Diagrams
Visual aids and diagrams are essential in an Achilles tendon rupture rehab exercises PDF guide. They help users understand proper exercise techniques, reducing the risk of improper form and injury. Include high-quality images or illustrations of each exercise, showing starting and ending positions. Diagrams of the Achilles tendon anatomy can educate patients about their injury. Use color-coded highlights to emphasize key movement areas. Incorporate before-and-after illustrations to demonstrate progress. Videos or animations, if possible, can provide dynamic instruction. Safety icons or warning symbols can alert users to common mistakes; Properly captioned visuals ensure clarity and enhance the guide’s effectiveness for diverse learners. Consistent styling improves readability and user experience.
7.3 Providing Clear Exercise Instructions
Clear exercise instructions are vital for a successful Achilles tendon rupture rehab program. Each exercise should be described with step-by-step guidance, including the starting position, movement sequence, and endpoint. Specify the number of sets, repetitions, and duration to ensure consistency. Use simple, jargon-free language to avoid confusion. Include tips on proper breathing, posture, and pacing to enhance safety and effectiveness. Provide visual cues or examples to clarify complex movements. Indicate when to progress or regress exercises based on individual tolerance. Emphasize the importance of gradual progression to prevent overexertion. Remind users to consult a healthcare professional if pain or discomfort arises during any exercise.

Monitoring Progress and Avoiding Reinjury
Regularly tracking healing milestones helps ensure a smooth recovery. Recognizing signs of overexertion, like pain or swelling, is crucial to avoid setbacks and reinjury.
8.1 Tracking Recovery Milestones
Tracking recovery milestones is essential to ensure progress and identify potential issues early. Regular assessments of pain levels, range of motion, and strength help gauge healing. Physical therapists often use standardized tools like goniometers to measure ankle mobility and dynamometers for strength testing. Patients should track their ability to perform daily activities and exercises without pain. Progress is typically monitored weekly or bi-weekly, with specific goals set for each phase of recovery. Achieving milestones, such as pain-free walking or resuming light activities, indicates readiness to advance to the next rehab phase; Consistent tracking ensures a tailored approach to rehabilitation, optimizing outcomes and minimizing delays.
8.2 Recognizing Signs of Overexertion
Recognizing signs of overexertion is critical to avoid setbacks in Achilles tendon recovery. Pain is a primary indicator—sharp, persistent, or increased pain during or after exercises signals potential overexertion. Swelling, redness, or bruising around the tendon area may also indicate excessive stress. Reduced mobility or stiffness in the ankle joint can be a warning sign, as can fatigue or weakness in the lower leg. If exercises become too challenging or cause discomfort, it’s important to pause and reassess. Consulting a physical therapist or healthcare provider is essential to adjust the rehab plan and prevent further injury. Monitoring these signs ensures a safe and effective recovery process.
8.3 Adjusting the Rehab Plan
Adjusting the rehab plan is essential to ensure progress and prevent plateaus or further injury. Regular assessments of strength, flexibility, and functional abilities help identify areas needing modification. If pain or swelling persists, exercises may need to be simplified or paused temporarily. Progression should align with individual recovery pace, avoiding rushing through phases. Incorporating feedback from physical therapists or healthcare providers ensures personalized adjustments. Lifestyle factors, such as activity levels or work demands, may also necessitate changes. A flexible approach promotes long-term success, ensuring the program remains challenging yet safe. Continuous monitoring and tailored adjustments are key to achieving full recovery and return to normal activities.
Role of Professionals in Rehab
Physical therapists, orthopedic specialists, and medical professionals play vital roles in guiding recovery, ensuring safe progression, and providing personalized care to achieve optimal outcomes in Achilles tendon rehab.
9.1 Physical Therapist’s Input
A physical therapist provides personalized guidance, creating tailored exercise plans to address specific recovery needs. They ensure proper technique, preventing reinjury and promoting optimal healing. Through manual therapy, pain management strategies, and progressive exercises, therapists enhance mobility and strength. Regular assessments track progress, adjusting plans as needed. Their expertise is crucial during initial healing phases, advancing to strengthening and functional movements. Collaboration with other professionals ensures comprehensive care, fostering a safe return to activity. A physical therapist’s input is vital for achieving long-term recovery and restoring full Achilles tendon function.
9.2 Orthopedic Specialist’s Guidance
An orthopedic specialist ensures the Achilles tendon heals correctly, offering expert advice on exercise progression and recovery timelines. They diagnose any structural issues and recommend surgical interventions if needed. By monitoring tendon integrity and patient response, they tailor rehabilitation plans to prevent complications. Their guidance is critical in managing chronic conditions and optimizing functional outcomes. Regular check-ups help assess healing milestones, ensuring safe transitions between rehab phases. The specialist’s input complements physical therapy, providing a holistic approach to recovery and enabling a successful return to activity.
9.3 Importance of Continuous Medical Supervision
Continuous medical supervision is essential to monitor healing progress, prevent complications, and ensure a safe return to activity. Regular check-ups allow early detection of issues like tendon re-rupture or improper healing. Adjustments to the rehab plan can be made promptly, optimizing recovery. Medical professionals provide personalized recommendations based on individual progress, ensuring adherence to established protocols. This oversight minimizes risks, accelerates recovery, and ensures the tendon achieves full strength and flexibility. Ongoing supervision also helps manage pain and inflammation effectively, promoting a smoother transition through each rehab phase and reducing the likelihood of long-term limitations. This comprehensive approach supports achieving the best possible outcome.
